Attempt to maintain health care Safety Net for low-income falters in state Legislature
 A campaign to protect a program helping lower-income people pay medical bills is facing opposition in the state Legislature and may not succeed. If lawmakers don’t block a bid by Gov. Charlie Baker’s administration to shrink the program, some lower-income patients and the hospitals that serve them – including Cambridge Health Alliance – could face heavier financial burdens, advocates of the program say.
A campaign to protect a program helping lower-income people pay medical bills is facing opposition in the state Legislature and may not succeed. If lawmakers don’t block a bid by Gov. Charlie Baker’s administration to shrink the program, some lower-income patients and the hospitals that serve them – including Cambridge Health Alliance – could face heavier financial burdens, advocates of the program say.
The governor plans to reduce income limits for the Health Safety Net program starting this month and eliminate the state contribution, now $30 million. His budget for the 2017 fiscal year beginning July 1 includes the cuts.
Last year about 274,000 people were enrolled in the program; advocates say the eligibility changes would affect almost 60,000 people.
Obamacare enrollment
The income limit for the program will drop to $72,250 from $97,000 for a family of four, and require more families and individuals to pay a deductible before benefits begin. State officials say almost all those who will lose benefits are eligible for subsidized insurance through the state’s Obamacare agency, the Health Connector, but haven’t enrolled despite rules requiring them to do so.
Supporters of the program generally don’t object to those requirements, but argue that many others in the Health Safety Net can’t pay medical bills even with Connector insurance or aren’t eligible for Health Connector coverage at all; elderly people who can’t afford to supplement their Medicare coverage, for example, were responsible for 20 percent of Health Safety Net bills last year, according to state figures.
Health Safety Net participants must get their care at a hospital or community health center, and supporters say the cuts will leave hospitals picking up more of the tab for patients who can’t afford to pay. Hospitals and insurers already pay $165 million to fund the program and hospitals alone are responsible for any shortfall. Last year, when the state contributed $30 million, the shortfall was $40 million; hospitals estimate it will be $100 million without state money.
Affecting Alliance
David Cecere, spokesman for Cambridge Health Alliance, the second-largest provider of care to the poor in the state, couldn’t say by the time this story was filed how the cuts will affect the hospital’s finances. The Alliance has said it expects to lose $13.1 million this year, but that figure could change.
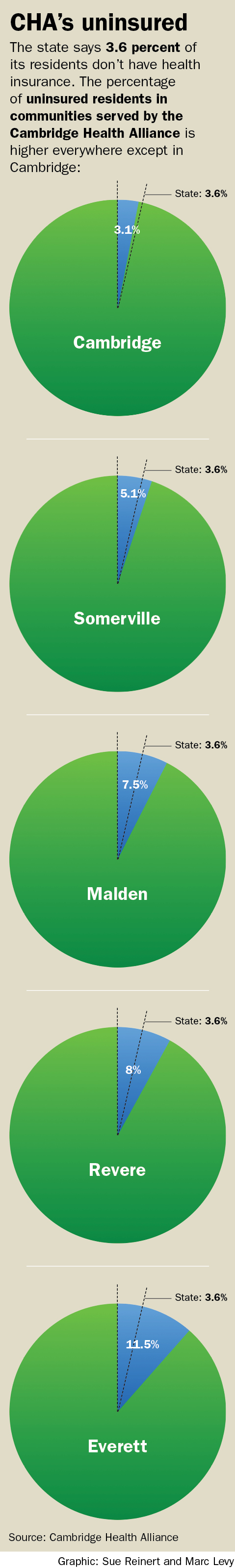
Earlier, Cecere provided figures on the percentage of uninsured residents in communities served by the Alliance: 11.5 percent in Everett; 8 percent in Revere; 7.5 percent in Malden; 5.1 percent in Somerville; and 3.1 percent in Cambridge. Except for Cambridge, the percentage of those without coverage exceeds the state figure of 3.6 percent last year.
The effort to keep eligibility limits unchanged got off to an inauspicious start when the state Senate failed to approve an amendment to this year’s budget that would have postponed the changes until June 30, the end of the fiscal year. The official date for the new limits is now today, but state officials have told hospitals and community health centers that they won’t fully enforce the changed eligibility standards until June 23.
In the Legislature

Barber
After that failure, lawmakers in the House didn’t approve an amendment filed by state Rep. Christine Barber, whose district includes Somerville, that would have preserved the program, including full state funding, in the 2017 budget.
State Sen. Jason Lewis of Winchester, a chairman of the Legislature’s Joint Committee on Public Health, filed the same amendment in the Senate. It was approved only after being changed to keep the eligibility limits for nine months, not the full year, and cut state funding to $15 million instead of leaving it at $30 million. A Senate staff member said Senate leaders wanted the shorter period and lower state funding.
The fate of the amendment is now up to a conference committee of six lawmakers from both houses that will resolve differences between the House and Senate budgets.
Step forward
Barber said in an email that Lewis’ amendment “does not get us to our final goal” but is still “a positive step forward” because it preserves current Health Safety Net standards for nine months and gives advocates a chance to “make a strong case” that the cuts will “harm vulnerable residents in our communities.”
The program, formerly called free care, was originally meant for people without health insurance. Since state health reform in 2003, the number of residents without coverage has fallen; last year 8 percent lacked insurance at least once during the year and 3.6 percent weren’t covered at the time of the state survey.
Still, undocumented immigrants, people with inadequate health insurance, seniors on Medicare and those with very high medical costs still need help, advocates say.


